#USA, August 13, 2022 – Cleveland Clinic has successfully performed a first-in-the-world full multi-organ transplant to treat a patient with a rare form of appendix cancer called pseudomyxoma peritonei (PMP). Upon completion of the lifesaving transplant surgery, the patient received five digestive organs: liver, stomach, pancreas, duodenum, and small intestine.
Anil Vaidya, M.D., Cleveland Clinic’s Intestinal Transplant Program co-director, led the seven-surgeon team that completed the pioneering operation on a 32-year-old man in September 2021.
“The patient had one of the more advanced cases of PMP I have seen,” said Dr. Vaidya. “While about 80% of patients with the condition can be treated with traditional therapies, what do you do with the 20% for whom the traditional therapy isn’t successful? In some cases, the answer may be a multi-organ transplant.”
with the condition can be treated with traditional therapies, what do you do with the 20% for whom the traditional therapy isn’t successful? In some cases, the answer may be a multi-organ transplant.”
During the 17-hour operation, surgeons removed the patient’s diseased organs. He then received the following deceased donor’s organs all together and at the same time: liver, stomach, pancreas and duodenum (pancreaticoduodenal complex), spleen, small intestine, and right colon. The donor spleen was initially transplanted to boost the immune protection of the newly transplanted organs and improve blood flow to the pancreas until fully transplanted. The donor right colon was initially transplanted to help protect the new intestine from infection and improve its ability to absorb nutrients. Both the donor spleen and donor right colon were removed prior to the completion of the transplant after they successfully served to protect the other organs during the operation.
“As far as we know, it is the first time in the world that a full multi-organ transplant, including the liver and four other digestive organs, is performed to treat PMP,” said Dr. Vaidya.
Prior to joining Cleveland Clinic in 2020, Dr. Vaidya performed in England the world’s first modified multi-organ transplant (excluding the liver) to treat a patient with PMP who had exhausted all other management strategies.
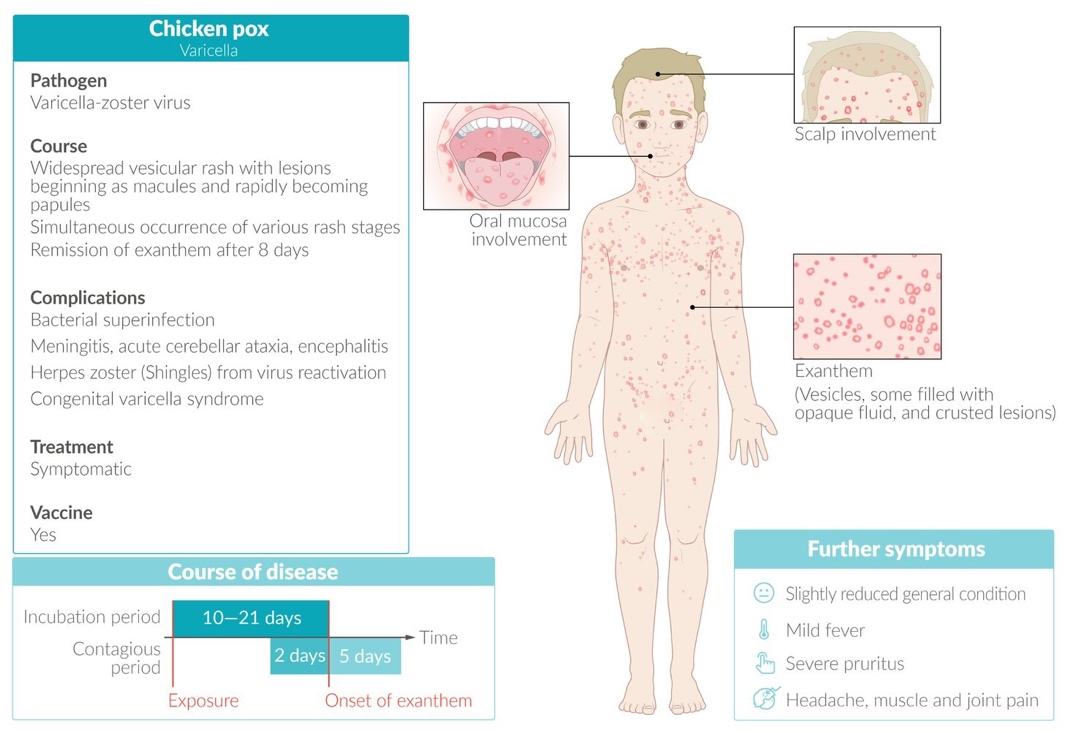
PMP is a rare cancer that typically originates as a tumor in the appendix. When the slow-growing tumor ruptures, its jelly-like content spreads to other digestive organs, with additional tumors developing that impair gastrointestinal function. Malnutrition and life-threatening complications ultimately occur.
Following the diagnosis in 2019, the patient began a long odyssey of treatments. He was one of the 20% of patients with PMP for whom the traditional treatments were ineffective. Often, this population of patients is left with few to no treatment options.
The patient was referred to Cleveland Clinic in 2021 in the end stage of his disease. He was receiving hospice care at that time. The patient had stopped working and could no longer eat solid foods. He was receiving nutrients intravenously through total parenteral nutrition (TPN).
“We needed to perform an evaluation to determine if transplantation in his case was safe, feasible and could provide long-term benefits,” said Dr. Vaidya.
Dr. Vaidya completed a thorough assessment of the patient’s case and received approval from Cleveland Clinic’s Intestinal Transplant Selection Committee to proceed. The patient was placed on the national transplant waiting list in July 2021.
“The patient – who needed a liver and four other digestive organs – had started to deteriorate quite rapidly,” said Dr. Vaidya. “It was touch-and-go that he would make it.”
In September 2021, a donor was found, and less than 24 hours later, the patient was undergoing the groundbreaking

surgery. The first three hours were preparatory, in essence removing the diseased abdominal organs. Next, the donor organs were inserted into the abdominal cavity, all the necessary vascular connections were completed and a left-sided ileostomy was created to handle bodily waste and let the body recover from the surgery.
“The operation was well planned and went like clockwork,” said Dr. Vaidya. “The team members knew exactly what they were going to do, and the timing was perfect. It went really well.”
Following the transplant, the patient remained in the hospital for 51 days. Soon after he was discharged, he returned because he was suffering from a case of graft-versus-host disease, a common occurrence following intestinal or bone marrow transplants where the donated organs’ immune cells recognize the recipient’s tissues as foreign and attack the recipient.
The patient underwent a procedure perfected and performed by Amy Lightner, M.D., colorectal surgeon and director of Cleveland Clinic’s Center for Regenerative Medicine and Surgery. Dr. Lightner administered three doses of mesenchymal stromal cell (MSC)-derived exosomes, a first ever, novel treatment in solid organ transplants — another first for a patient who received a full multi-organ transplant to treat PMP.
According to Dr. Vaidya, “The patient’s recovery was absolutely amazing. His symptoms abated within two hours of the first dose.”
Nine months post-transplant, the patient, now 33, can eat and digest solid foods again and has energy to do what he loves, including walking and biking outdoors.
“There is currently no evidence of cancer recurrence,” said Dr. Vaidya.
Photo Captions:
Header: Masato Fujiki, MD, (center) and the Cleveland Clinic surgical team, led by Anil Vaidya, MD, performing the first-in-world multi-organ transplant to treat a rare type of appendix cancer. (Photo courtesy of Cleveland Clinic)
1st insert: Anil Vaidya, M.D.
2nd insert: From left: Anil Vaidya, M.D., Shannon Jarancik, physician assistant, Amy Lightner, M.D., Andy Voge, patient, Rachel Voge, Andy’s wife, and Anita Barnoski, transplant coordinator.
Release: Cleveland Clinic / DPA media


 TCI News1 week ago
TCI News1 week ago
 Latin America and Caribbean1 week ago
Latin America and Caribbean1 week ago
 Bahamas News1 week ago
Bahamas News1 week ago
 Crime1 week ago
Crime1 week ago
 Bahamas News6 days ago
Bahamas News6 days ago
 Caribbean News1 week ago
Caribbean News1 week ago
 Bahamas News6 days ago
Bahamas News6 days ago
 Caribbean News1 week ago
Caribbean News1 week ago