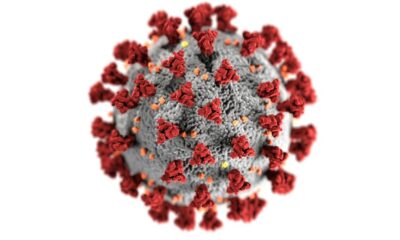
Port of Spain, Trinidad and Tobago. 5 July 2024. Mosquito borne diseases continue to pose a serious public health threat to the Caribbean Region. The Caribbean Public Health Agency (CARPHA) has increased reports of Dengue outbreaks with hospitalisations and deaths in some instances, and recently confirmed cases of Zika, and Chikungunya at its Medical Microbiology Laboratory.
These mosquito-borne diseases can have a major impact on our way of life and our vital tourist industry on which most of our islands depend.
“The Region of the Americas has seen a two-hundred-fold increase in suspected Dengue cases in the first half of 2024, compared to the same period in 2023. Member States are encouraged to remain vigilant. It is crucial that surveillance, prevention and control measures are boosted to reduce the transmission of arboviruses in the Caribbean,” stated Dr. Lisa Indar, Ad Interim Executive Director at CARPHA.
Dengue is known to cause outbreaks every three to five years. The Region has seen outbreaks of Chikungunya and Zika virus infections that challenged public health systems in virtually every country in our Region.
Dr. Horace Cox, Assistant Director of Surveillance, Disease Prevention and Control, and Head Vector Borne Diseases at CARPHA: “These viral infections are transmitted by the Aedes aegypti mosquito – a vector known to be endemic to the Region. With the start of the hurricane season CARPHA is urging its Member States to strengthen integrated vector management strategies in their communities. These include the elimination of mosquito breeding sites with the aim of reducing the number of mosquito larvae.”
To counter the increase in mosquitoes and potential disease transmission, greater effort should be placed on mosquito control activities in communities, and these should be intensified. CARPHA urges its Member States to review their preparedness and response plans, as well as to continue surveillance, early diagnosis, and timely care of arboviral disease cases, to prevent complications leading to hospitalisation and deaths.
Mr. Rajesh Ragoo, Senior Technical Officer for Vector-Borne Diseases at CARPHA stated “Community involvement is essential in the fight against mosquito-borne diseases. A proactive approach can help to reduce risk and keep communities safe.”
- Check and remove standing water from around your home. Ensure your surroundings are clean and free of materials or containers that can accumulate water around your homes and communities.
- Use of wire-mesh/screens on doors and windows also help in reducing the entry of mosquitoes into homes.
- Water storage drums and tanks must be properly covered and inspected periodically to ensure that there is no breeding. Roof gutters should also be cleaned to prevent water from pooling.

The mosquitoes that spread dengue are active during the day. Personal preventative measures to minimise mosquito bites are also extremely important. Vulnerable groups such as infants, young children, older adults, and women who are pregnant, or trying to get pregnant, must be extra cautious. Long-sleeved clothing and repellents containing DEET, IR3535 or lemon eucalyptus, should be used to protect exposed skin, and must be used in accordance with the instructions on the product label. Confirmed cases of mosquito borne diseases should rest under mosquito nets.
CARPHA remains committed to supporting CARPHA Member States (CMS) in their vector control efforts, including capacity building in integrated vector control strategies. CMS must continue to strengthen prevention and control measures such as surveillance, diagnosis, as well as timely and adequate treatment of cases, while ensuring that health care services are prepared to facilitate access and proper management of patients with these diseases.
CARPHA has produced campaigns to raise awareness, promote effective prevention, and control measures for mosquito borne diseases. Information about mosquito borne diseases can be found here:


 Caribbean News1 week ago
Caribbean News1 week ago
 Caribbean News7 days ago
Caribbean News7 days ago
 Caribbean News1 week ago
Caribbean News1 week ago
 Caribbean News1 week ago
Caribbean News1 week ago
 Bahamas News7 days ago
Bahamas News7 days ago
 News7 days ago
News7 days ago
 Bahamas News1 week ago
Bahamas News1 week ago
 News7 days ago
News7 days ago