Providenciales, Turks and Caicos Islands, 4th January 2024 - Since the beginning of the dengue outbreak in the TCI, the MOH has identified 172 cases of dengue. These cases include cases confirmed through testing at the Caribbean Public Health Laboratory (90) as well as cases identified locally through the use of dengue rapid tests. The cases are distributed as follows:
167 Providenciales
5 Grand Turk
Dengue virus types were established for 76 out of the 90 laboratory confirmed cases. Seventy-four (74) laboratory confirmed cases were type 3 and 2 were type 2 Dengue. Type 3 dengue is associated with more severe disease.
A total of 18 persons with dengue have been hospitalized. There have been no reports of any dengue related deaths.
Age groups affected are primarily 20-59 years age group followed by 6-19 years. The most affected communities in Providenciales are Blue Hills followed by Five Cays.
A greater proportion of males, 60.5% (n=104) were detected with dengue when compared to females with 37.8% (n=65) (for the remainder, no gender was documented).
Dengue is a viral illness that spreads to people through the bite of an infected Aedes species (Ae. aegypti or Ae. albopictus) mosquito. These mosquitoes also spread zika, chikungunya, and other viruses. The aedes aegypti mosquito is present in the Turks and Caicos Islands and is capable of spreading these diseases. The Aedes aegypti prefers to lay their eggs in artificial containers that contain water (drums, barrels and tires, mainly) in and around homes, schools and workplaces. It is essential that the general public remains vigilant for this disease as well as play their role in destroying potential mosquito breeding sites within homes, yards and communities.
as play their role in destroying potential mosquito breeding sites within homes, yards and communities.
- 1 in 4: About one in four people infected with dengue will get sick.
- For people who get sick with dengue, symptoms can be mild or severe.
- Severe dengue can be life-threatening within a few hours and often requires care at a hospital.
Symptoms
- Mild symptoms of dengue can be confused with other illnesses that cause fever, aches and pains, or a rash.
- The most common symptom of dengue is fever (40°C/104°F) with any of the following:
- Nausea, vomiting
- Rash
- Severe headache
- Aches and pains (eye pain, typically behind the eyes, muscle, joint, or bone pain)
- Any warning sign
Symptoms of dengue typically last 2–7 days. Most people will recover after about a week.
Individuals who are infected for the second time are at greater risk of severe dengue.
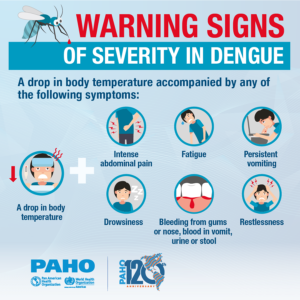
Severe dengue symptoms often come after the fever has gone away:
- severe abdominal pain
- persistent vomiting
- rapid breathing
- bleeding gums or nose
- fatigue
- restlessness
- blood in vomit or stool
- being very thirsty
- pale and cold skin
- feeling weak.
People with these severe symptoms should get care right away. 
There is no specific treatment for dengue. If you suspect that you or your loved one has dengue, please see your healthcare provider so you can be tested and receive the necessary advice. Avoid taking non-steroidal anti-inflammatory drugs, like ibuprofen and aspirin.
Persons who are suspected to have dengue or have confirmed dengue should avoid further mosquito bites.
The Ministry of Health and Human Services continues to offer testing for dengue at no cost through the National Public Health Laboratory in partnership with the Caribbean Public Health Agency (CARPHA) as well as conducting vector control activities throughout the islands.
Prevention and control
The mosquitoes that spread dengue are active during the day.
Lower the risk of getting dengue by protecting yourself from mosquito bites by using:
- clothes that cover as much of your body as possible
- mosquito nets if sleeping during the day, ideally nets sprayed with insect repellent
- mosquito repellents (containing DEET, Picaridin or IR3535)
- during the first week of infection, dengue virus is found in the blood of an infected person. If a mosquito bites
 the infected person, the mosquito becomes infected. The infected mosquito can spread the virus to other people through bites. Infected persons should therefore avoid being bitten.
the infected person, the mosquito becomes infected. The infected mosquito can spread the virus to other people through bites. Infected persons should therefore avoid being bitten.
- use screens on windows and doors. Repair holes in screens to keep mosquitoes outdoors.
- stop mosquitoes from laying eggs in or near water.
- once a week, empty and scrub, turn over, cover, or throw out items that hold water, such as tires, buckets, planters, toys, pools, birdbaths, flowerpots, or trash containers.
- check for water-holding containers both indoors and outdoors.
- ensure tight coverage of water barrels, containers and water storage tanks
Response
The Ministry of Health and Human Services has been responding to the threat posed by dengue by;
- the implementation of the Integrated Vector Management Plan throughout the islands with efforts to reduce mosquito breeding through the use of larvicide and fogging which only targets the adult mosquito population
- vector control activities including premises inspections, have resulted in a reduction in some areas of mosquito breeding
- the EHD has been working with stakeholders across sectors to address mosquito breeding including Tourism, Ports/Airports, Pest Control Operators, Schools, Hospitals, airlines etc.
- visits were conducted to schools across the islands which included inspections and provision of educational talks to students about dengue and how they could help prevention efforts
- public education/community engagement campaign has been ongoing utilizing public service announcements, radio interviews, social media and leaflets is ongoing to educate to general public about the critical role each person plays in reducing mosquito breeding through keeping the environment free of debris as well as avoiding mosquito bites, the importance of getting tested as well as education on the warning signs of dengue which would need early medical intervention. Additional information can be found on the Health Promotion and Advocacy Units Facebook page https://www.facebook.com/tcihealthpromotions/.
- the Environmental Health Department has also been working closely with its regional and international stakeholders including PAHO (Pan American Health Organization), CARPHA (Caribbean Public Health Agency) and UK Health Security Agency (UKHSA). Through a number of technical visits including visits by Entomologists and training provided to Vector Control Unit staff, the response has been reviewed and refined.
- material resources including chemicals have been procured and distributed across the islands
- temporary vector control officers have been approved and have joined the team to support operations
- community clean ups have been ongoing aimed at reducing mosquito breeding sites
All of these measures have seen a reduction in the number of persons presenting to health care facilities with symptoms of dengue.
There have however been recent rains which can result in mosquito breeding.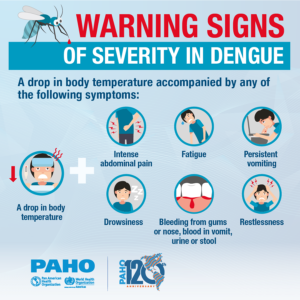
The public plays a key role in preventing the further spread of dengue and they are being urged to;
- Ensure that water barrels and buckets are properly covered to prevent mosquito larvae,
- Cover or properly dispose of old tires,
- Properly dispose of all litter and waste. These overlooked breeding grounds perpetuate the cycle of dengue transmission.
Prevention through ensuring clean environments, sanitation, and public awareness, with active community involvement is crucial to supporting the Ministry’s response to dengue.
The public is also reminded to report any areas of standing water or mosquito breeding sites by contacting the Environmental Health Department for assistance on (649) 338 2143/2142.

 Crime2 days ago
Crime2 days ago
 TCI News2 days ago
TCI News2 days ago
 Latin America and Caribbean1 week ago
Latin America and Caribbean1 week ago
 Bahamas News1 week ago
Bahamas News1 week ago
 Bahamas News1 week ago
Bahamas News1 week ago
 Bahamas News1 week ago
Bahamas News1 week ago
 Bahamas News20 hours ago
Bahamas News20 hours ago
 Bahamas News2 days ago
Bahamas News2 days ago